There are so many reasons why some people dread the Holiday season. Let’s explore the list as it is not the same for everyone and feel free to add your comments about other ways you find helpful to get through the Holiday season.

SOLUTIONS Cancer Resource Center, Inc.
Empowering patients to be actively engaged in their cancer care
There are so many reasons why some people dread the Holiday season. Let’s explore the list as it is not the same for everyone and feel free to add your comments about other ways you find helpful to get through the Holiday season.

We recently entered the season where the daylight savings time has caused us to turn our clocks back an hour to adjust to the longer days without the sun, and in comes SAD. Seasonal Affective Disorder (SAD) is a type of depression that occurs seasonally, primarily during the fall and winter months. This condition can significantly impact a person’s mood, energy levels, and overall well-being. While the exact cause of SAD is not fully understood, it is believed to be linked to reduced exposure to sunlight and changes in the body’s internal clock.

Let’s take a good look at the symptoms
Symptoms of SAD can vary from mild to severe and may include:
How do we cope?

While SAD can be challenging, there are effective strategies to manage its symptoms. There is light therapy that can help regulate your body’s internal clock and improve your mood. Have you considered engaging in physical activity. Take a brisk walk, turn on YouTube find a yoga class – it has proven to boost your energy levels and reduce feelings of depression. In addition, practices like meditation, mindfulness, and deep breathing can help reduce stress and anxiety. Consider spending time with loved ones and participating in social activities can alleviate feelings of loneliness and isolation. The diet is also key, eating a balanced diet rich in fruits, vegetables, and whole grains can support your overall well-being.

However, if symptoms are severe, consider seeking professional help from a mental health professional. They can provide therapy, medication, or a combination of both to manage SAD effectively. The ultimate goal is to discover ways for individuals with SAD to improve their quality of life and navigate the challenges of the darker months.
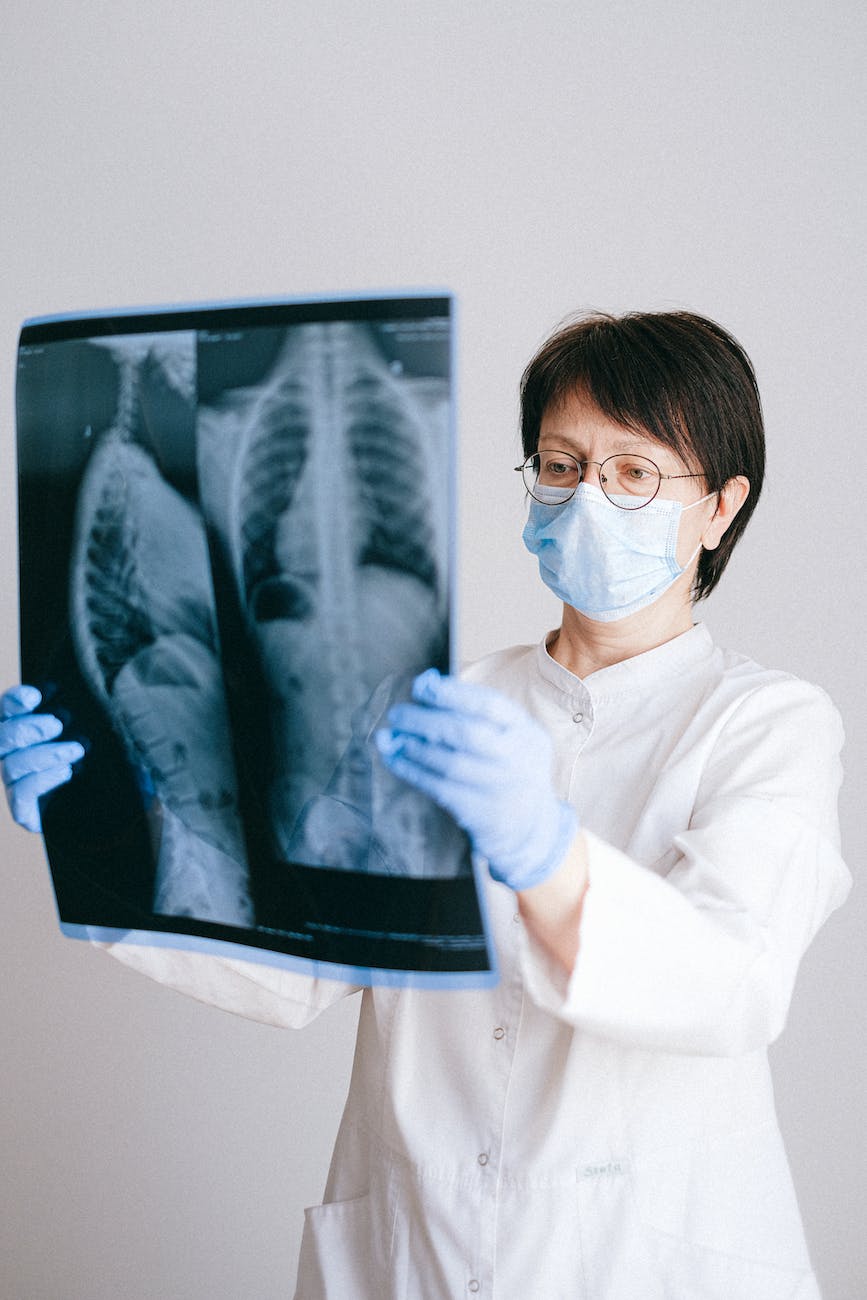
Today, as we observe World Lung Cancer Day, it is imperative to shed light on this formidable disease. Lung cancer, often insidious in its onset, remains a leading cause of cancer-related deaths globally. The disease disproportionately affects specific demographics, underscoring the importance of targeted prevention and early detection efforts.
Symptoms of lung cancer can be subtle and often mimic those of common ailments, making early detection a challenge. A persistent cough, chest pain, shortness of breath, and blood in sputum are among the most common indicators. However, it’s crucial to remember that these symptoms can also be attributed to other conditions. Therefore, regular check-ups and prompt medical attention for any persistent or unusual symptoms are vital.

Smoking remains the primary risk factor for lung cancer. Yet, it’s essential to dispel the myth that only smokers are at risk. Exposure to secondhand smoke, radon, asbestos, and certain chemicals can also increase the likelihood of developing this disease. This underscores the importance of comprehensive public health strategies to address both smoking cessation and environmental factors.
Treatment options for lung cancer have advanced significantly in recent years, including surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy. Early detection significantly improves the chances of successful treatment. Therefore, raising awareness, promoting early screening, and encouraging healthy lifestyle choices are critical steps in combating this deadly disease.

World Lung Cancer Day serves as a poignant reminder of the importance of prioritizing lung health. By understanding the risks, recognizing the symptoms, and advocating for early detection, we can work towards a future where lung cancer is no longer a leading cause of death.
*References:
World Health Organization. (n.d.). Lung cancer. Retrieved from https://www.who.int/news-room/fact-sheets/detail/lung-cancer
American Cancer Society. (n.d.). Lung Cancer. Retrieved from https://www.cancer.org/cancer/types/lung-cancer/about.html
National Cancer Institute. (n.d.). Lung Cancer Treatment (PDQ®)–Patient Version. Retrieved from https://www.cancer.gov/types/lung/hp

Life, it seems, is a relentless teacher. Over the years, the lessons etched into my soul have not come from textbooks, but from the raw experiences of serving within my community. My journey began with a fervent mission – to educate about the importance of early detection through cancer screenings and preventive measures. Countless workshops, community forums, and one-on-one conversations fueled my belief that knowledge was power in the fight against this relentless disease.
Yet, a stark reality emerged. Most encounters were with those already facing the storm, diagnosed with cancer, often at an advanced stage. This realization stung. The very people I aimed to empower were coming in when options dwindled. It ignited a new passion within me – to be the steadfast presence for families navigating the treacherous waters of diagnosis, treatment, and hospitalization.

My role is being the expert, the advocate, the one who deciphered medical jargon and guided through baffling bureaucratic hurdles. Yet, the weight of that role became painfully evident when my brother succumbed to cancer just four weeks and four days after his diagnosis. The feeling of failure, the helplessness, lingers to this day.
But grief, it turned out, was not the endpoint. Instead, it fueled a fierce determination in my approach to my sister, burdened by the same family history. Here, vigilance became my mantra. Early detection, constant monitoring, a proactive approach – these became the cornerstones of our fight. This journey emphasized the importance of empowering patients and families to be active participants in their own healthcare. It is not just about information; it is about ownership, about feeling heard and understood.
Despite advancements in research and treatment, the harsh truth remains – minority communities grapple with disproportionately high cancer mortality rates. This disparity is unacceptable. My voice echoes not only within the community, but also in the halls of research institutions and government offices. I am a bridge between the battlefield of disease and the architects of solutions. I advocate for affordable, accessible healthcare, for increased funding for research, and for a system that truly serves the needs of all.
The lessons continue to unfold. Serving my community isn’t just about offering knowledge or navigating the healthcare system. It’s about advocating for change, for a world where early detection truly empowers, where the advancements in research touch all lives, not just some. This is the fire that burns within me, a fire that compels me to be the voice for those who have not found theirs, a voice echoing in the halls of power and whispering alongside patients as they chart their course.
The fight continues.

In the grand orchestra of life, their instruments are often silent, their melodies subtle, yet their impact resonates through the ages. They are the caregivers, the quiet warriors who stand beside us, holding hands and whispering encouragement through life’s storms. Today, we raise our voices in appreciation, singing a hymn to their unwavering dedication.
Caregivers are not defined by a title or a profession. They are mothers and fathers, daughters and sons, spouses and friends, neighbors and strangers. They are the lighthouse keepers in the storms of illness, the steady hands guiding through darkness, the unwavering hearts offering solace in despair.
Their days are rarely filled with applause or accolades. They rise before dawn, their bodies heavy with the weight of responsibility, yet their spirits kindled by a love that knows no bounds. They bathe, feed, and comfort, offering not just physical care but also emotional support, a listening ear, and a quiet strength that whispers, “You are not alone.”

Their nights are often fragmented, punctuated by the cries of need, the anxieties of their loved ones mirrored in their own hearts. Yet, they rise again, fueled by an unwavering dedication, their exhaustion a badge of honor worn silently, their love a shield against fatigue.
Caregivers are witnesses to the fragility of life, the bittersweet dance of joy and sorrow. They hold hands with those who walk through the valley of the shadow, their presence a beacon in the darkness, their love a testament to the enduring power of the human spirit.
But caregivers are not just givers; they are also receivers. They receive the love and gratitude that shines through the eyes of their loved ones, the unspoken words that speak volumes of appreciation. They receive the strength that comes from knowing they are making a difference, that they are weaving threads of hope into the lives they touch.

So, today, let us pause and celebrate these unsung heroes. Let us acknowledge the sacrifices they make, the burdens they carry, and the love they pour out so generously. Let us offer our thanks, our support, and our understanding, for they are the silent anchors in our lives, the quiet heroes who remind us of the true meaning of love and compassion.
This hymn is for them, the unsung heroes who walk beside us, reminding us that even in the darkest hours, the human spirit can shine brightly. Thank you, caregivers. You are the light that guides us through life’s journey.
Resources
Find support through these organizations
The National Alliance for Caregiving https://www.caregiving.org
Family Caregiver Alliance: National Center on Caregiving https://www.healthinaging.org/tools-and-tips/family-caregiver-alliance-national-center-caregiving
National Family Caregivers Association https://caringcommunity.org/resources/models-research/national-family-caregivers-association-nfca/
American Caregiver Association https://americancaregiverassociation.org/

It was the first Sunday of the New Year! Awakened by an intense pain, she knew she would not make it to church. It was much too much. She had to get to the hospital, her husband got the car. It was very early, still dark, the sun had not yet appeared. In fact, the forecast of a snow storm was expected that day. The drive to the Emergency Department brought a great sense of relief as the pain would be taken care of.
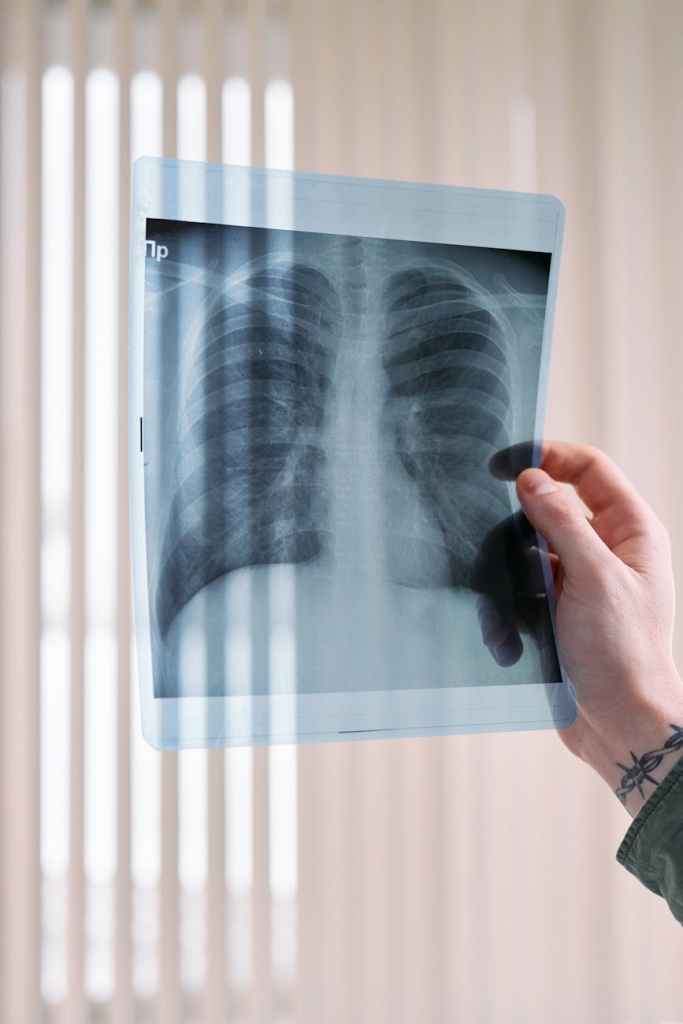
The sterile white walls of the emergency room seemed to hum with fluorescent light, amplifying the thudding rhythm of Stephanie’s heart. Her back, the culprit of her visit, throbbed a dull counterpoint. But it was the doctor’s words, echoing in the sterile air, that truly stole her breath: “Two small nodules on your lung” the words echoing in the cavernous space of her skull. Small, he’d said. But the word echoed like a thunderclap, each syllable reverberating with uncertainty.
Stephanie, ever the pragmatist, had nodded politely, the news seemingly bouncing off her carefully constructed shield of composure. She’d asked clarifying questions, her voice betraying no hint of the tremor in her hands.
She’d come for the back pain, a nagging ache that had morphed into a sharp, unwelcome guest. But the CT scan, meant to reveal kidney stones or a pinched nerve, had unearthed something far more unsettling. Nodules. The word hung heavy, its weight threatening to crush the carefully constructed facade of calm she’d presented to the doctor.
In the quiet solitude of the examination room, the mask slipped. The ache in her back was forgotten, replaced by a chilling emptiness in her chest. Two nodules. What did they mean? Were they shadows, harmless wisps on her scan, or ominous portents of something worse?
Her mind, once a whirlwind of deadlines and errands, became a hurricane of possibilities. Images flashed, each one a grimmer echo of the last: needles glinting in sterile hands, hushed voices in sterile hallways, waiting rooms filled with the ghosts of unspoken anxieties.

The doctor’s reassurances, delivered with practiced optimism, felt like whispers in a storm. “Further tests, of course,” he’d said, “but try not to worry.” Try not to worry. Easier said than done when the future seemed to stretch before her, a vast, uncharted ocean, dotted with the treacherous reefs of “what ifs.”
She forced a smile for the nurse. The world outside seemed to have muted its colors, the vibrant reds and greens of the city park across the street replaced by a monochrome palette of fear.
The hours that followed were an eternity of waiting, of stealing glances at the clock, of replaying the doctor’s words in her head like a broken record. Each creak of the door, each hurried step in the hallway, sent her heart into a frantic dance.
But amidst the fear, a flicker of defiance. This wasn’t the end. Not yet. She would face this, this unwelcome shadow lurking in her lungs, with the same grit she’d faced every other challenge life had thrown her way.
She closed her eyes, picturing her grandmother and mother, recalling the foundation of faith, their prayers and resilience. They faced many challenges throughout their lives. “Life is a tapestry, Stephanie,” mother once said, her voice dramatically animated, “woven with threads of joy and sorrow, light and dark. But it’s up to you to choose the color of the final stitch.”
And so, Stephanie chose defiance. She would weave this thread, this dark, unexpected thread, into the tapestry of her life. It wouldn’t define her, wouldn’t erase the vibrant colors of her past or dim the possibilities of her future. It would be a challenge, a hurdle, but one she would face with courage, with hope, with the unwavering belief that even in the shadow of uncertainty, the final stitch could still be a thread of light.
As the day seemed over, the dark dreary clouds created a complete covering of the sky, as though it aligned with the unexpected news of the day. Taking a short walk to the car, still in pain, the earlier hopes of leaving the Emergency Department with some relief were dashed. Stephanie felt a shift within her. The fear was still there, a cold ember in her chest, but it was no longer the only thing she felt. There was defiance, a quiet resolve, a determination to weave this unexpected thread into a story of resilience, of facing the unknown with courage and grace.
The doctor’s referral would bring answers, some definitive, some shrouded in the grey fog of further tests. But for now, Stephanie found solace in the quiet strength that had risen within her. She would face this, she would fight, and she would, one stitch at a time, weave a tapestry of hope, even in the shadow of two small, ominous nodules.

November is Pancreatic Cancer Awareness Month, and out comes the bullhorn as I take this opportunity to be a part of the campaign. True to form, like a broken record, I share my very personal experience with the disease. It was summer, August of 2018, three days after his birthday, my brother was diagnosed with pancreatic cancer. Four weeks and four days later, he was gone.
So, what is pancreatic cancer? Pancreatic cancer is a cancer that starts in the pancreas, a gland that produces digestive enzymes and hormones. It is one of the most aggressive and deadly cancers, with a five-year survival rate of just 10%. However, early detection can improve survival rates significantly.

Early Detection
There is no specific screening test for pancreatic cancer, but there are some things that people can do to increase their chances of early detection, such as:
Symptoms
The symptoms of pancreatic cancer can be vague and often mimic other conditions, such as gastritis or pancreatitis. This can make it difficult to diagnose early on. However, some of the most common symptoms of pancreatic cancer include:
If you experience any of these symptoms, it is important to see a doctor right away.

Diagnosis
If a doctor suspects that you may have pancreatic cancer, they will likely order a number of tests, including blood tests, imaging tests, and a biopsy.
Treatment Options
The treatment options for pancreatic cancer depend on the stage of the cancer, the patient’s overall health, and their personal preferences. Some of the most common treatment options include:

Progress in Research
There has been significant progress in pancreatic cancer research in recent years. For example, scientists have identified new genetic markers that can help to diagnose pancreatic cancer earlier. They have also developed new drugs and treatment strategies that are showing promise in clinical trials.
Targeted therapy drugs target specific molecules that are involved in the growth and survival of cancer cells. This type of therapy is often more effective and has fewer side effects than traditional chemotherapy drugs. Furthermore, immunotherapy drugs help the body’s own immune system fight cancer cells. Immunotherapy is a relatively new type of treatment for pancreatic cancer, but it has shown promising results in clinical trials.
Resources for Patients and Families
There are a number of resources available to support patients with pancreatic cancer and their families. Some of these resources include:
Pancreatic cancer is a challenging disease, but there is hope. With early detection and treatment, more and more people are surviving pancreatic cancer. Cheers to the survivors. Prayers of hope for those who are diagnosed and are currently in treatment. Prayers of comfort for the families who have lost a loved one.

The Right to Die is a controversial topic that has been debated for many years. There are many different opinions on this issue, and it is important to consider all of the challenges, controversies, and benefits before making a decision. It may be referred as death with dignity, or assisted suicide.
One of the main challenges of the Right to Die is that it can be difficult to determine when a person is truly ready to die. Some people may feel like they are ready to die when they are in pain or when they are no longer able to live independently. However, others may feel like they are ready to die when they are simply tired of living. It is important to make sure that a person is truly ready to die before they make a decision to end their life and thankfully, there are systems in place to ensure that the individual patient is well informed and has received the proper counseling.

Another challenge of the Right to Die is that it can be difficult to ensure that a person’s wishes are carried out. If a person decides to end their life, they may want to make sure that their family and friends are aware of their decision. They may also want to make sure that their doctors are aware of their decision so that they can provide them with the necessary assistance. However, it is not always possible to ensure that a person’s wishes are carried out.
The Right to Die is also controversial because it can be seen as a form of suicide. Suicide is a serious issue, and it is important to make sure that people who are considering suicide are getting the help they need. However, it is important to remember that the Right to Die is not the same as suicide. The Right to Die is a decision that a person makes about their own life, and it is not something that is forced upon them. The individual is weighing what they consider is best for them in their own journey through life – all the way to the end.
As of March 8, 2023, physician-assisted suicide is legal in 11 US states and the District of Columbia. These states are:
In addition to these states, physician-assisted suicide is also legal in the Netherlands, Belgium, Luxembourg, Switzerland, Canada, and several countries in South America and Europe.
The laws governing physician-assisted suicide vary from state to state and may be monitored by a nurse as the patient takes the medication on their own. In general, however, patients must be mentally competent, terminally ill, and have a prognosis of six months or less to live. They must also request physician-assisted suicide on two separate occasions, at least 15 days apart.
Physician-assisted suicide is a controversial issue, and there are strong arguments both for and against it. Those who support physician-assisted suicide argue that it gives terminally ill patients the right to control their own death and to die with dignity. They also argue that it can help to alleviate suffering and that it can be a more humane alternative to prolonged illness and death.

Those who oppose physician-assisted suicide argue that it is morally wrong to help someone to kill themselves. They also argue that it can lead to abuse, and that it can send the message that life is not worth living if it is not free of pain and suffering.
The right to die is a complex issue with many challenges, controversies, and benefits. Some of the challenges include:
Some of the controversies surrounding the right to die include:
Some of the benefits of the right to die include:
People who are terminally ill or who are suffering from a debilitating condition may want to end their lives so that they can die on their own terms and alleviate the long suffering as their family and friends gather around for visits. The patient is already overwhelmed with the process of dying and struggling with the idea of being a burden. The Right to Die can also give people the peace of mind knowing that they have the option to end their lives if they choose.
Above all, have compassion for those who are making those difficult decisions. Be grateful and hopeful that you nor your loved ones would ever have to consider such a life altering option.

At this point, the years are swiftly coming and leaving us to figure out where it went and how we can ensure that this year we will be able to maximize our time. While some may make resolutions, list their goals and create vision boards, which by the way I have certainly done, I have adjusted to working on my goals until they are completed.

Here is a list of things that we should all do this year –
Cheers to the quote “If it is to be, it is up to me.” – William Johnsen
Go Forth!
A Powerful Health Benefit – Meditation


♪♪Tis the season to be jolly♪♪
It is that time of the year as we are reminded through the songs, the smiling faces, the decorations, the gifts and all of the parties. While, the atmosphere is in a festive mood, sadly not everyone is sharing in the joy of the season. There are families who are having a tough time during the jubilant season.
This may be the first time that everyone is gathered to spend the day as they always do except that there is something different this time, someone is obviously missing. The loss may be from a divorce, separation, military deployment, illness or death. Whatever the reason, it can affect the mood of those who are facing the holidays without their loved one.
The first Thanksgiving without my father was difficult as he was the family chef during the holidays. Our mother cooked all of the meals throughout the year – Thanksgiving and Christmas was a feast on another level. We considered having our dinner catered. We just wanted to gather together and have dinner and spend our time together as a family. While we were grateful for the years we shared with our father, we were in the midst of mourning all that he meant to us especially on a day where we looked forward to his delicious spread.

In the case where your loved one is in the hospital, nursing home or rehabilitation facility, perhaps a visit will cheer everyone up. It will definitely make your loved one feel better knowing that they are not forgotten..

Remembering the good times is key. Memories may deliver a mixture of emotions. One moment there may be tears as you wish that your loved one could be with you all, while the next moment may be filled with laughter as you recall the happy times. Laughter is the best medicine, I know this for sure, laughter has helped us through some very tough times during the holidays. It sure takes adjusting especially in the cases where there is a permanent loss.

There is a saying ‘Time heals all wounds’ which it does. However, it takes time – some longer than others. The best way to cope is to acknowledge your feelings then allow yourself to embrace the transition of understanding that while life will never be the same, your life must go on.